Hidden in Plain Sight: Are You Enrolled in Medicaid Without Knowing It? A Guide for Tennessee Residents

Navigating health insurance can be confusing, especially when the name doesn't quite match the service. In Tennessee, and across several other states, a surprising trend is emerging: health insurance plans are being offered that functionally operate as Medicaid, but without explicitly using the term “Medicaid.” This can leave enrollees unaware of the program's specifics, potential limitations, and how it might be affected by changes in federal policy.
Why the Name Game?
States employ this tactic for a variety of reasons. Some believe that the term “Medicaid” carries a negative stigma, potentially deterring eligible individuals from enrolling. Others argue it's a marketing strategy, aiming to present a more appealing image than the traditional Medicaid branding. Whatever the motivation, the practice obscures the true nature of the coverage.
How Does It Work?
These plans, often referred to as “alternative benefit plans” or “managed care organizations,” are contracted by the state to administer Medicaid services. They receive funding from the state's Medicaid program and are required to provide a similar scope of benefits. However, the branding and marketing materials often downplay or omit the connection to Medicaid.
What Tennessee Residents Need to Know
If you have health insurance in Tennessee, it's crucial to understand whether it's actually Medicaid in disguise. Here's what you should be aware of:
- Eligibility Requirements: Medicaid eligibility rules apply, regardless of the plan's name. Income, residency, and other factors still determine your qualification.
- Benefits Covered: The plan should cover the same essential health benefits as traditional Medicaid. Verify this by reviewing your plan documents and contacting the provider.
- Provider Network: Confirm that your preferred doctors and hospitals accept the plan. Managed care plans often have specific provider networks.
- Appeals Process: Understand how to appeal denied claims or coverage decisions. The Medicaid appeals process typically applies to these plans as well.
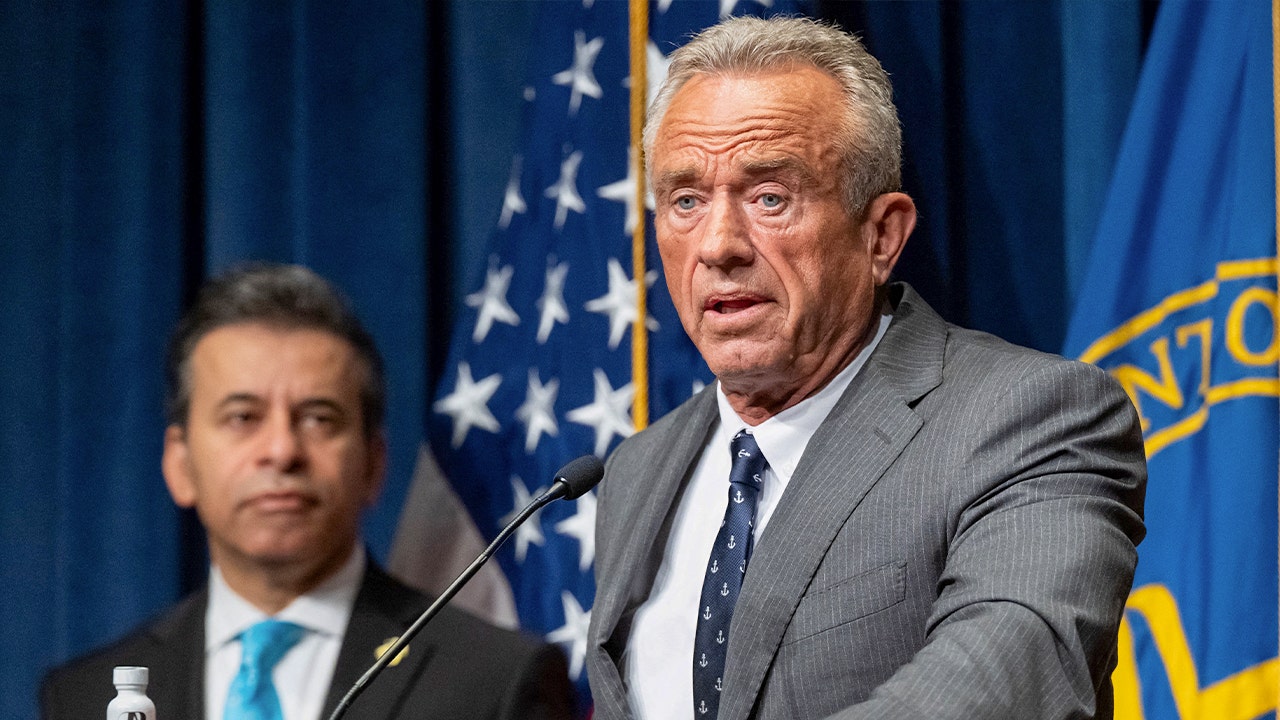
- Federal Policy Changes: The potential impact of federal policy changes, such as those related to the Affordable Care Act or Medicaid funding, remains a significant concern. Trump's “Big Beautiful Bill” and subsequent policy shifts have created uncertainty for Medicaid recipients nationwide. These changes could impact funding, eligibility requirements, and the scope of covered benefits. Staying informed is essential.
The Implications of Federal Policy
The current political climate adds another layer of complexity. Federal legislation could significantly alter the Medicaid landscape, potentially impacting states that have adopted these alternative benefit plans. Changes to federal funding or eligibility requirements could affect the availability and affordability of healthcare for vulnerable populations. It’s vital to stay updated on these developments and understand how they might impact your coverage.
Protecting Your Healthcare Access
Don't let confusing names obscure your healthcare rights. Take the time to understand your health insurance plan, confirm its connection to Medicaid, and stay informed about relevant policy changes. Resources are available to help you navigate this complex system:
- Tennessee Medicaid Website: [https://www.tn.gov/health/topic/medicaid](https://www.tn.gov/health/topic/medicaid)
- Healthcare.gov: [https://www.healthcare.gov/](https://www.healthcare.gov/)
- Local Advocacy Groups: Contact organizations that advocate for healthcare access in Tennessee.
By being proactive and informed, Tennessee residents can ensure they receive the healthcare coverage they deserve, regardless of what their plan is called.